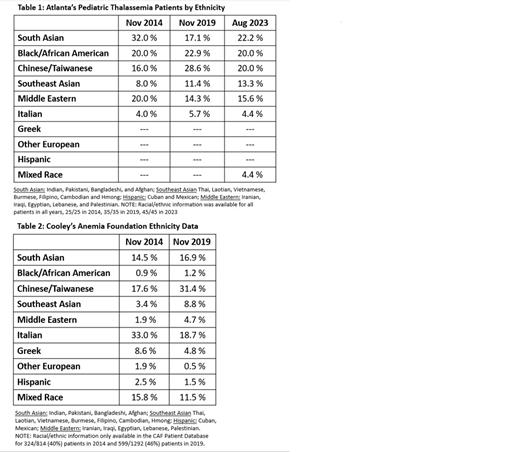
Thalassemia is a common disorder worldwide but remains relatively rare in the United States (U.S). Over the past decade, there has been a significant demographic shift as more patients are entering care as either international adoptees or refugees from under-resourced countries. We analyzed our own center's demographic evolution from 2014 to 2023. Only transfusion dependent thalassemia (TDT) patients fully managed within our pediatric center are represented in Table 1. We did not include non-transfusion dependent thalassemia (NTDT) patients nor TDT patients who have graduated to adult care, relocated, or those who travel to our center only for comprehensive visits from out of state. When compared to the national data collected by the Cooley's Anemia Foundation (CAF), we saw a similar increase in patients from China and Southeast Asia (SEA), reflecting the increased number of adoptees in the period from 2014-2019 (Tables 1 & 2). Since that time, we have seen an increase in patients from South Asia (SA) and the Middle East (ME). These patients are mostly refugees from regional conflicts (Syria, Afghanistan, Myanmar, etc.). This trend is similar to other centers, according to the CAF (unpublished communication).
Interestingly, however, our center has a significantly larger proportion of Black TDT patients compared to the national data (Table 2 ). As can be seen in the tables below, we have nearly 20x more Black patients (20-22.9% vs. 0.9-1.2%) when compared to the national data. This may be in part due to our center's location in Atlanta, Georgia. However, according to the latest U.S. Census data, Georgia's population is 33.1% Black, compared to 13.6% in the U.S population as a whole. Based on this, we would expect a 2.4x increase, as opposed to a 20x increase. Vichinsky et al published a study in Pediatr Blood Cancer in 2017 using data collected from 4 Comprehensive Thalassemia Treatment Centers (CTTC) in the Northeast, Midwest and West coast of the U.S. looking at the racial distribution and changes of NTDT patients. They also found a higher-than-expected proportion of Black patients, about 17%. Of our 65 NTDT patients, 26% are Black and an additional 5% are mixed race, Black and Asian. The majority (60%) have Hemoglobin H disease. We looked to see if our TDT patients were relatives of sickle cell disease (SCD) patients, since our center has the largest pediatric SCD population in the U.S. However, only 20% (2/10) report family members with any form of SCD. The majority (8/10) of the patients identify as African American, whereas the remaining 2 are 1st generation Somalian and Ghanaian. Genotype data is available for 9/10 patients, with three ß0/ß0 and six ß+/ß0. The most common mutations seen were IVS II-849 A>G (ß0), -29nt A>G (ß+), Promoter -88nt G>T (ß+) and Codon 5 (-CT) frameshift (ß0). All are mutations predominantly found in Blacks. Clinically, as a group, they had a high rate of splenomegaly (8/10) and skull changes (6/10) before transfusions began. Transfusions began ages 6mos-9 yrs. with 50% occurring after age 3 yrs. Black TDT patients may face unique challenges in the U.S. where there are >50 SCD patients for every thalassemia patient. Indications for transfusion and overall clinical management are vastly different for these two diseases, but providers with little experience in the treatment of Thalassemia may inappropriately treat them like SCD patients.
Disclosures
Boudreaux:BlueBirdBio: Other: Advisory Board; Vertex: Other: Advisory Board; BMS,BristolMyersSqibb: Other: Advisory Board. Tang:NovoNordisk: Research Funding; Pfizer: Membership on an entity's Board of Directors or advisory committees, Research Funding. Graciaa:Agios: Other: Advisory Board.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal